Background: Patients with B cell acute lymphoblastic leukemia (B-ALL) relapsed after allogenic hematopoietic stem cell transplantation(alloHSCT) have poor prognosis and the median survival after relapse was 4 - 5.5 months, estimated 2-year post-relapse survival rates were 10 - 16%. Donor lymphocyte infusion (DLI) have shown limited success in the setting of relapse by a mere increase in median survival by 6 months and a significant risk of acute and chronic graft-versus-host disease (GVHD) and additional risk of marrow aplasia. The donor chimeric antigen receptor-T cell (CAR-T) for CD19 is a promising treatment for relapsed and refractory B-ALL, but the effectiveness and safety of donor-derived CD19 CAR-T cell infusion for relapsed B-ALL after alloHSCT have not been determined.
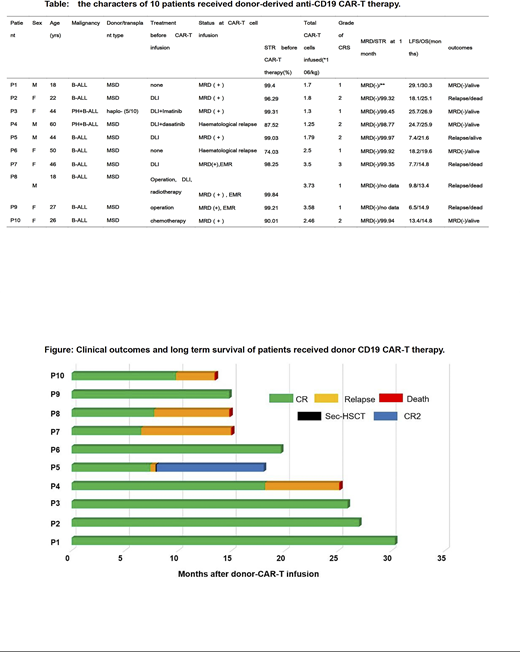
Methods: Between July 2017 and Nov 2018, 10 adult patients with B-ALL relapsed (4 patients were hematologic relapsed, 3 patients were extramedullary relapse, the other 3 patients were bone marrow MRD-positive, Table) after alloHSCT were enrolled, including 9 sibling-matched stem cell transplantation and 1 haploidentical transplantation. About 100 - 200 ml venous blood form each donor was obtained and the T cells were separated. Then donor's T cells were infected with lentivirus carrying CD19 CAR plasmid which containing CD19 scfv (HI-19 clone) and 4-1BB-CD3ζ signaling domains to generate CAR-T cells. ALL the 10 Patients received FAC (fludarabine: 25-30mg/m2/d*3, cyclophosphamide:350mg/m2/d*2, cytosine arabinoside:100mg/m2/d*4) pretreatment and then a total of 5.01 × 106/kg (range, 3.39 - 6.53 × 106/kg) donor T cells including donor-derived anti-CD19 CAR-T cell (1.82 × 106/kg, (range, 1.26 - 4.67 × 106/kg)) was infused on 2 or 3 consecutive days for each patient. The levels of cytokines including IL-1,IL-2R,IL-6,IL-8,IL-10 and the percentage of the donor anti-CD19 CAR-T cells were monitored serially . Clinical manifest and the severity of cytokine release syndrome (CRS) were recorded and evaluated. The bone marrow examination was performed every 2 weeks after CAR T-cell infusion to assess the response for the first 2 months and then was performed every 1-3 months including bone marrow smear, MRD detection by flow cytometry, fusion gene detection by quantitative real-time polymerase chain reaction (qPCR), donor chimera rate by short tandem repeat(STR).
Results: The median transduction efficiency of the final donor-derived CD19 CAR-T cells was 35.8%(range 25 - 70.6%). The peak of donor-derived anti-CD19 CAR-T cell expansion in the recipients was about 7 - 14days after infusion and then decreased rapidly. The serum cytokines levels varied differently: the serum IL-6 and IL-2R levels increased overtly and reached the peak during day 5 - day 7 in most of the patients, whereas the serum levels of IL-1, IL-8 and IL-10 did not vary obviously. one patient experienced Grade 3 CRS, 4 patients experienced Grade 2 CRS and the other 5 patients only experienced Grade 1 CRS. Four patients showed encephalopathy and 2 patients received glucocorticoid treatment. All the 10 patients achieved MRD negative remission and complete donor chimerism within 14days to 42days after donor's CAR-T cells infusion. No patients developed acute or chronic graft-versus-host disease (GVHD). After a median follow-up of 20.6 months (range, 13.4-30.3), 5 patients (including all the 3 patients with extramedullary relapse) relapsed with leukemia cells CD19-dim and 4 of them died due to disease progression. Only one patient received a successful secondary alloHSCT from a haplo-identical donor. The other 5 patients showed persistent complete donor chimerism with MRD negative remission(Figure). The estimated 2-year overall survival and leukemia-free survival were 68.6% and 48.0%, 2.5-year OS and LFS were 51.4% and 48.0%.
Conclusion: Donor-derived CD19 CAR-T cell infusion seems to be an effective and safe treatment for B-ALL relapsed after alloHSCT, especially for those without extramedullary disease, which may be confirmed with more clinical studies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.